HOME >> CHINA
Chinese virologists urge longer isolation for discharged COVID-19 patients retesting positive
By Wang Qi Source:Global Times Published: 2020/4/1 20:58:40
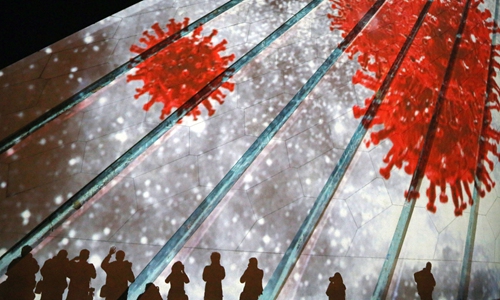
File Photo: AFP
New research shows that young and mild COVID-19 patients appear to be retested positive after being discharged and they show no obvious clinical symptom and disease progression upon re-admission. Some virologists called for prolonged isolation and detailed observation for discharged patients while using high-sensitive detection kits as much as possible.
Called "Clinical characteristics of the recovered COVID-19 patients with re-detectable positive RNA test," the preprint article was published on medRxiv by Chinese researchers from Shenzhen 3rd People's Hospital, National Clinical Research Center for Infectious Disease, and Translational Research Center under Tsinghua University.
The paper says researchers studied 262 COVID-19 patients discharged from January 23 to February 25 this year. They were categorized into two groups: re-detectable positive patients, or RP patients, and non-RP (NRP) patients, and were tested using high-sensitive detection methods.
The study revealed that the vast majority of RP patients (97.4 percent) were under 60 years old. Among them, patients younger than 14 were more common compared with those between the ages of 14 and 60 years old. All 38 RP patients recovered from mild and moderate conditions, and after they tested positive and were re-admitted to the hospital, they showed no obvious clinical symptoms and disease progression, nor did their 21 close contacts.
China's top epidemiologist Zhong Nanshan disclosed last month that some experts from the University of Hong Kong studied over 10 RP patients and did not culture live virus from samples, suggesting that the element that triggered the positive reading might be the virus fragment, which is not infectious.
Yang Zhanqiu, a Wuhan-based virologist, told the Global Times Wednesday that although no close contacts were found infected, it cannot prove that the RP patients were non-infectious due to the limits of observation. And the phenomena of re-detectable positives must be given serious attention.
"Re-detectable positive tests could point to a false negative, which means that the patient has yet to recover, and might also be caused by environmental contamination like clothes and rooms, or the kit itself, or just the inaccuracy of the test due to the kit or the medical workers' operations."
Yang said the age might not be a key factor as different samples may lead to different results. Normally speaking, patients who recovered from a severe condition are most likely to retest positive, as they carried higher doses of the virus but recovered slowly. However, the results of the study might suggest that the virus is deceptive to the immune system of mild patients, which failed to kill the virus completely.
The research also suggested the significance of more accurate test kits, which are able to improve the detection of residual virus and avoid a possible "false negative" due to low-sensitive commercial RNA detection kits.
In the latest study, for samples from 15 RP patients who were sampled after 5-7 days since the onset of the re-admission, eight of them were confirmed positive using the hyper-sensitive kit, while only one person was confirmed using the commercial kit.
Yang said that although it is great to have the high-sensitive kit widely used to increase accuracy, hospitals face problems like costs, the more complicated operation, and a longer time for results.
Besides the high-sensitive kit, the expert suggested that promoting the standardization of testing is also important, involving the standardization of testing ways, sampling operations, and kit quality from various manufacturers.
Yang noted that supervision is also important, and suggested prolonging the duration of isolation and observation after the patients are discharged from the hospital, as well as strengthening the supervision of the close contacts of RP patients.
Posted in: SOCIETY